The Nipah virus has become a major public health threat in recent years. This zoonotic pathogen specialized in Southeast Asia has produced various outbreaks and serious disease and death. The dynamics of the Nipah virus crisis need to be understood for proper prevention and control. However, the virus is particularly challenging because it is so fatal and potentially widespread. Its impact is deemed so important that governments and health organizations worldwide are focusing on research and response strategies to overcome this. While management of the crisis depends greatly on public awareness and education, it is important to understand that we are, as always, in this together.
Why Awareness is Critical to Public Health
Public health is safeguarded with awareness about the Nipah virus. People living in educated communities are more aware of Nipah virus symptoms, undertake preventive measures, and bring down the risks for transmission. It can debunk myths and misinformation, which are spread through awareness campaigns and create a more informed and resilient population. By this, the vulnerable population gets access to the right information required on time, and timely interventions are helped as well through effective communication strategies. Also, awareness efforts help healthcare providers to identify and treat the disease early, resulting in better patient outcomes. An awareness-based approach to dealing with accidents ensures that societies can become better equipped to defend themselves from the Nipah virus and other emerging infectious diseases.
Understanding Nipah Virus
What is the Nipah virus?
The henipavirus genus that the Nipah virus is part of is highly infectious. Primarily, it infects humans and animals; the diseases that result are very severe respiratory and neurological diseases. The virus was discovered in 1998 during an outbreak in Malaysia and has since then been found in some Asian countries. Nipah virus infections may cause mild symptoms but can also range to acute encephalitis, leading to high mortality. Its potential for human-to-human transmission and its lack of a widely available vaccine make the virus a Level 4 biosafety pathogen. Control measures will be effective if we understand its biology and transmission pathways.
History of the Nipah Virus: When and Where It BeganThe Nipah
The virus was first identified in 1998 in an outbreak among pig farmers in Malaysia. Initially, the cases were accompanied by severe respiratory and neurological symptoms, and over a million pigs had to be culled to try to contain the spread. The disease has also reemerged in Bangladesh, India, and elsewhere in Southeast Asia. Every outbreak has given us important lessons regarding how this virus is transmitted and how it affects people. Historical evidence shows that the virus can ‘jump’ from animals to humans and is sometimes helped by environmental and social factors. To better predict future outbreaks and be prepared for them, studying past outbreaks is important.
How the Virus is Classified: A Look at the Henipavirus Family
The Henipavirus family includes both the Hendra virus and the Nipah virus. These single-stranded RNA viruses are enveloped and highly pathogenic. Henipaviruses are zoonotic, and natural reservoirs are fruit bats. This family is classified according to genetic and structural similarities and pathogenic characteristics. Classification facilitates determining the potential for cross-species transmission risks as well as helping to design targeted antiviral therapeutics. Ongoing research into hepatitis viruses reveals their intricate relationships with a host and with the environment.
Global Spread: Countries and Regions Most Affected
More than 20 countries in South and Southeast Asia have been affected by the Nipah virus. In the late 1990s, several outbreaks had been observed in Malaysia and Singapore. Repeated cases have been reported almost annually in Bangladesh, associated with the ingestion of contaminated date palm sap. Sporadic outbreaks have also occurred in India, mostly in the northeast of the country. Deforestation, urbanization and changes in agricultural practices all play a role in how the virus spreads. Global travel and trade can help spread the virus across borders, reinforcing the strength of international cooperation in surveillance and response.
Transmission of Nipah Virus
Zoonotic Origins: Animals That Spread the Virus
Fruit bats of Pteropus species are the primary reservoir for the Nipah virus. The virus lives in these bats without any symptoms and functions as its natural carrier. Humans have usually contracted infection through contact with infected bats or their secretions. Furthermore, the virus moves through intermediate hosts, such as pigs, and amplifies in larger outbreaks. Less frequently, other animals—such as horses and cats—have been implicated. Preventing spillover events and controlling the spread of the virus requires us to understand zoonotic transmission pathways.
Human-to-Humann Transmission: How It Happens
The Nipah virus can be spread from human to human through close contact, directly with the infected individual or through contact with their bodily fluids. This mode of transmission is particularly worrying in healthcare settings where poor infection control practices prevail. Human transmission is primarily droplet transmission, salvia, and other secretions. Prolonged exposure puts caregivers and family members at greater risk. Strict hygiene protocols and protective measures are paramount in stopping the transmission of the virus and preventing outbreaks.
Environmental Factors Contributing to Spread
Nipah virus transmission is heavily dependent upon environmental factors. Natural ecosystems are disrupted by deforestation and habitat destruction that accelerate contact between human and wildlife reservoirs, such as fruit bats. Bat migration patterns can change and expand regions of virus spillover with climate change. For example, bat secretions can become contaminated in agricultural practices, e.g., in the cultivation of date palm sap. These interactions exacerbate urbanization and population growth, necessitating an approach to sustainable environmental management aimed at reducing the risk of transmission of the disease.
Role of Fruit Bats in Nipah Virus Outbreaks
Nipah virus ecology is built on fruit bats. The virus lives asymptomatically in their bodies, and they can transmit it through oxen, droppings, and saliva. Then, the bats can contaminate food sources, like fruits and date palm sap, that humans can eat without knowing they are contaminated. Their wide-ranging flight patterns allow the virus to be spread over large geographic areas. Prevention strategies include protecting bat habitats and reducing human-wildlife interactions. Avoiding contact with bat-contaminated resources is further public education that mitigates transmission risks.
Risk Factors for Nipah Virus Infection
Several risk factors are present in Nipah virus infection. Exposure risks escalate in contact with infected individuals, in particular in healthcare settings. Those most vulnerable are occupations that involve working with animals, for example, pig farming. In certain regions, consumption of raw date palm sap contaminated by bats is a main transmission route. Higher infection numbers are mainly due to poor sanitation and a lack of awareness about preventive steps. Targeted interventions towards these risk factors can greatly lower the incidence of Nipah virus infection.
Early Signs of Nipah Virus
Recognizing Nipah Virus Symptoms Within the First Week
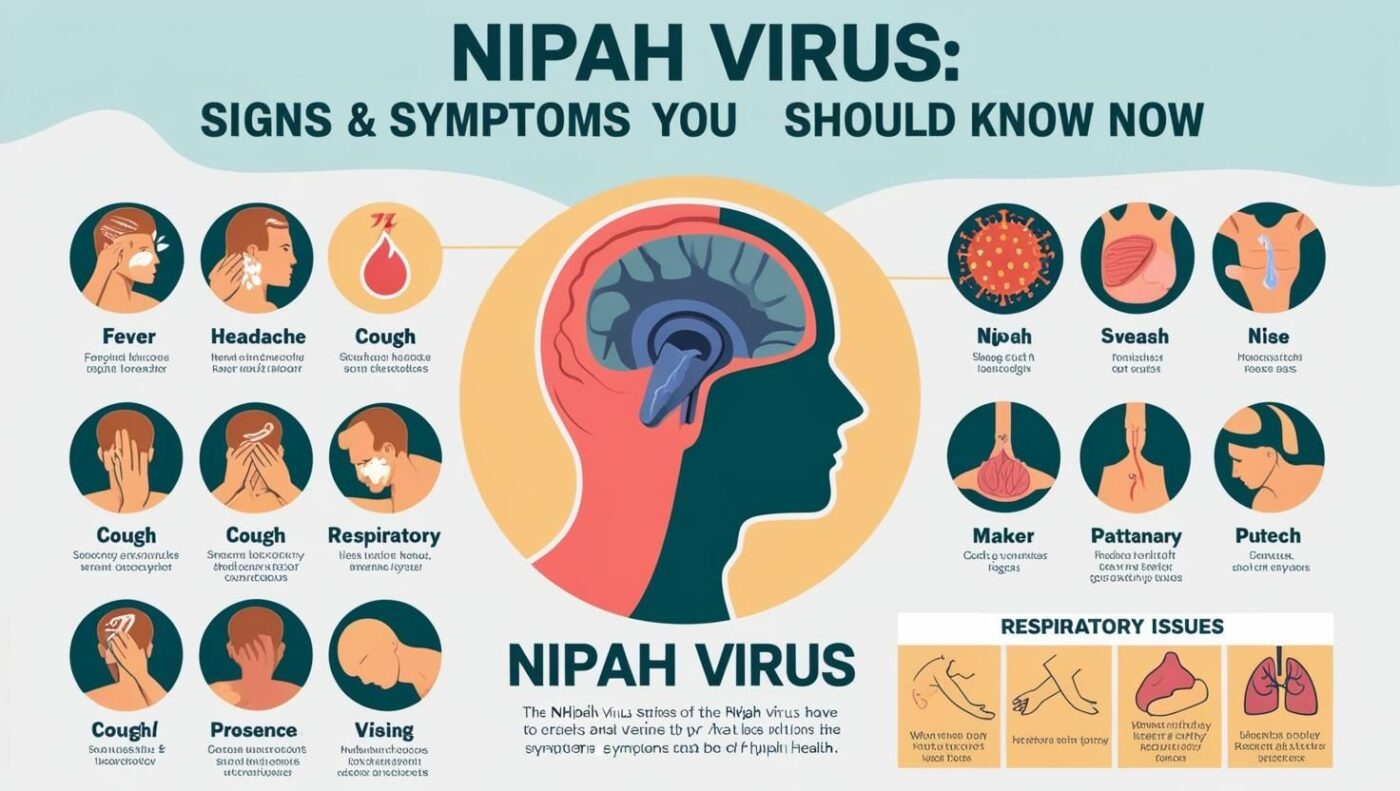
Early detection of Nipah virus infection is effective management and containment for Nipah virus infection. Signs and symptoms usually begin five to 14 days following the exposure. Signs often start nonspecific, mimicking the common cold, thus delaying diagnosis. Early and timely medical checkups are recommended and can help protect other people. In outbreak-prone areas, healthcare providers are key to the identification of potential cases.
Fever and Headaches: Common Initial Indicators
The initial symptoms of Nipah virus infection are most often fever and headaches. These are Nipah virus symptoms of the body’s response to the immune system’s invasion of a virus. Headaches may range from mild to severe, and fever may be persistent and high. Early indicators such as these are critical in initiating additional medical evaluation, particularly in those with known exposure risk. Early diagnosis and treatment may improve patient outcomes when fevers or headaches are presented early.
General Weakness and Fatigue
Those infected with the Nipah virus also feel weak and tired, with fever and headache. These Nipah virus symptoms indicate how the virus affects the entire body. It exhausts individuals, making daily tasks challenging. Other symptoms, such as muscle aches and joint pain, can worsen when fatigued, making for a complicated clinical picture. Knowing these signs will help you start supporting care measures early enough.
Severe Symptoms of Nipah Virus
Respiratory Distress and Breathing Problems
In severe cases of the Nipah virus, the infection can progress until causing respiratory distress and breathing difficulties. Symptoms may include patients being short of breath more rapidly; they may breathe rapidly, and they may decrease oxygen levels. ARDS can evolve to an acute stage and requires intensive medical intervention, including mechanical ventilation. Respiratory symptoms significantly elevate mortality risk and need urgent medical care to maintain lung function and avoid further complications.
Symptoms: Seizures, Confusion, and Drowsiness
In people, the Nipah virus can cause severe neurological diseases, including seizures, confusion, and drowsiness. The result is inflammation and damage from the virus invading the central nervous system. In severe cases, confusion and drowsiness can progress to coma, and seizures can be recurrent and difficult to control. The clinical management of patients is complicated by neurological involvement, including brain inflammation, from which the patients need specialized care to prevent long-term damage.
Encephalitis: Brain Inflammation and Its Effects
Encephalitis, or brain inflammation, is one of the most severe complications of a Nipah virus infection. It abnormalities of normal brain function cause symptoms such as severe consciousness and motor dysfunction. If the inflammatory response leads to swelling and increased intracranial pressure, it can be quite hazardous to neurological health. Many people with encephalitis have a poor prognosis, and treating encephalitis depends largely on aggressive medical treatment aimed at reducing inflammation and supporting the function of the central nervous system.
Signs of Critical Illness: Warning Signs to Watch
Critical illness in Nipah virus infection is a rapid deterioration of health. Warning signs of a critical illness include persistent high fever, respiratory distress, seizures, and loss of consciousness. According to these indicators, medical intervention and intensive care are required urgently. Timely recognition of these signs can aid in treatment, avoiding the spread of the virus in healthcare facilities and communities and saving lives.
Diagnosing Nipah Virus

Tests Used to Identify Nipah Virus Infection
Nipah virus infection is diagnosed through clinical assessment and laboratory tests. RT-PCR (reverse transcription polymerase chain reaction) is the principal diagnostic technique for detecting viral RNA in blood, cerebrospinal fluid, or respiratory samples. Serological tests seek antibodies to the virus generated by exposure, whether prior to or during the infection. Specialized laboratories also use immunohistochemistry and virus isolation. Effective patient management relies on an accurate and timely diagnosis, which in turn leads to outbreak control.
Common Challenges in Diagnosis
The Nipah virus is difficult to diagnose. Its early symptoms are nonspecific and can mimic other viral infections, leading to misdiagnosis. Diagnostic facilities in outbreak-prone regions are limited, and testing is delayed. Furthermore, high-level biosafety laboratories are needed to perform this testing, limiting the availability of capabilities. Patient care is also inadequate; transmission risks increase due to diagnosis delays, highlighting the need for improvement in diagnostic infrastructure and training.
Differentiating Nipah Virus From Other Diseases
Differentiation of the Nipah virus from other potential pathogens with similar clinical presentations is required for a prompt diagnosis and subsequent management. Overlapping symptoms, such as fever, headache, and neurological disturbances, apply to Japanese encephalitis, rabies, and influenza, all of which are contagious diseases. The Nipah virus must be diagnosed because of the importance of its differentiation from these diseases, for which molecular and serological tests are important. Differentiation of disease in a timely and accurate manner enables appropriate medical interventions to take place and avoid unnecessary treatment to help achieve better patient outcomes and outbreak management.
Role of Rapid Response in Accurate Diagnosis
Nipah virus diagnosis and containment require a fast response. This allows suspected cases to be identified quickly, and supportive care can be provided immediately. By enabling rapid testing capabilities to confirm infections, public health measures can be taken to prevent further spread quickly. Effective coordination between healthcare providers, laboratories, and public health authorities is essential to minimizing the impact of infectious disease outbreaks.
Complications of Nipah Virus

Long-Term Neurological Effects
Nipah virus infection can have long-term neurological effects in survivors, including cognitive impairments, memory loss, and motor dysfunction. The virus can also cause encephalitis, and leaving the condition untreated can lead to lasting brain damage, limit a person’s ability to function daily and affect their quality of life. Often, rehabilitation services are needed to assist patients in gaining and adapting to these challenges. Since it is important to understand and respond to long-term effects, care for survivors should be comprehensive.
Respiratory Failure and Its Impact
The severe Nipah virus is often complicated by respiratory failure. It happens when the lungs do not deliver enough oxygen to the body, and the body’s organs start to have problems ‘working’ due to hypoxemia. At times, breathing support in these patients may necessitate mechanical ventilation, but not all patients respond favorably to interventions. The mortality risk and burden of clinical management of infected individuals are greatly enhanced by respiratory failure, emphasizing the requirement for maximizing respiratory support in the critical care setting.
Fatal Outcomes and Survival Rates
The Nipah virus has a very high human mortality rate, usually more than 70 percent. Serious respiratory and neurological complications are usually fatal. Survival rates are affected by how soon medical treatment is provided, how well supportive care is delivered, and whether there are other health conditions. Survival chances are best in patients whose disease is detected early and treated aggressively, but prognosis is often quite poor in many cases. Work continues to find effective treatments and vaccines to decrease mortality.
Prevention of Nipah Virus
Importance of Personal Hygiene in Virus Prevention
Maintaining personal hygiene is important to prevent the transmission of the Nipah virus. Regular handwashing with soap and water eliminates viral particles, reducing the risk. Raw fruits that may have been contaminated with bat secretions must be avoided. Personal protective measures, such as gloves and masks, also help minimize exposure risks. Promoting hygiene practices can greatly improve communities.
Avoiding Close Contact With Infected Individuals
To prevent human-to-human transmission of the Nipah virus, close contact with infected people must be avoided. Transmission is best reduced by isolating infected persons and providing them with the right medical care. When connecting with patients, caregivers and family should wear protective equipment, and all should follow strict hygiene protocols. According to public health guidelines, outbreaks are best contained, and vulnerable populations are protected by minimizing direct contact.
Safe Practices Around Animals
Safe handling of animals is very important for controlling the Nipah virus. If you work with animals, particularly pigs or bats, use protective gear and avoid direct contact with infected animals or their secretions. Proper sanitation and biosecurity measures can reduce zoonotic transmission in animal husbandry. Spillover events can be mitigated by educating communities to engage safely with wildlife and livestock in a way that benefits human and animal health.
Protecting Food Supplies From Contamination
Preventing the contamination of the food supply protects against the Nipah virus. Fruits (and other consumables) should also be free of bat droppings and secretions. Pasteurizing dates, palm sap, and other ingredients can remove viral particles from high-risk foods. Implementing food safety standards, monitoring our supply chains and ensuring that the virus does not enter the human food supply can reduce the risk of becoming infected.
Using Protective Gear: Masks and Gloves
People at risk for exposure to Nipah virus should use protective gear, including masks and gloves. Masks are worn so that you don’t breathe respiratory droplets that have the virus, and gloves because you’re trying not to touch the contaminated surface or material. Usage of personal protective equipment (PPE) is mandatory in healthcare settings to protect healthcare workers from getting infected with COVID-19 and subsequently to protect patients from having a healthcare worker themselves with COVID-19. Effective virus transmission prevention needs proper training on the use and disposal of PPE.
Role of Healthcare Professionals

Managing Nipah Virus Patients in Hospitals
As the Nipah virus patients are managed in hospital settings, healthcare professionals have a big role in the management. Patient management involves timely diagnosis, isolation, and supportive care for respiratory and neurological symptoms. Strict infection control procedures help to control the spread of nosocomial transmission. Keeping a safe and effective treatment environment requires that healthcare workers are trained in recognizing symptoms and how to handle infected patients.
Guidelines for Healthcare Workers’ Safety
Good Nipah virus outbreak control requires adherence to guidelines on the safety of healthcare workers. One example of these guidelines is the appropriate use of protective personal equipment (PPE), regular hand hygiene, and proper handling of biological specimens. Procedures must be developed for the isolation of suspected cases and the management of waste to avert environmental contamination by these facilities. Monitoring and continuous training ensure that healthcare workers are always protected against infectious diseases and receive the most current infectious control information.
How Rapid Testing Helps Control the Spread
Controlling the spread of the Nipah virus requires rapid testing. Information on the decedent is provided to the health department, which can then verify death by providing the truth of the prognosis and date of death to a funeral home within hours in order to facilitate funeral arrangements. Quick initiation of supportive care is achieved with rapid tests that help improve patient outcomes. They also help public health authorities track and respond to outbreaks efficiently. Rapid diagnostic technologies represent great investment opportunities to increase the ability to contain and manage Nipah viral infections quickly.
Vaccination and Treatment

Current Status of Nipah Virus Vaccine Development
A Nipah virus vaccine is of global public health importance. Several candidate vaccines are in various degrees of research and development to elicit strong immune responses to the virus. The results of preclinical studies have been promising, but large-scale clinical trials are needed to demonstrate safety and efficacy. Achieving this will require additional collaboration and constitute a responsibility shared by multilateral organizations, governments, and research institutions to accelerate vaccine development and ensure broad, equitable access when available.
Supportive Care Options for Infected Patients
The primary mode of treating Nipah virus infections is supportive care. This includes keeping the patient well hydrated, giving the patient oxygen if respiratory distress occurs, and treating the neurological effects of encephalitis and seizures. However, patients with severe symptoms, such as those who require mechanical ventilation and renal support, require intensive care units (ICUs) when necessary. Early and aggressive supportive care will improve survival rates and lessen the severity of complications associated with the virus.
Investigational Therapies in Use Today
Therapies to reduce viral replication and alleviate symptoms attributable to Nipah virus infections are currently being investigated. In experimental settings, antiviral drugs, including ribavirin, have some efficacy; however, in clinical use, this remains uncertain. Potential for targeted treatment is also being investigated using monoclonal antibodies targeting the virus. However, these therapies must be proven effective in clinical trials and research studies before they are validated and integrated into standard procedures.
The Importance of Quarantine Measures
Measures of quarantine are important in restraining the Nipah virus outbreak. Human-to-human transmission of the virus stops when we isolate the infected individuals and thus control the spread within the communities. Quarantine practices like restricting one’s movement, providing medical care, and watching over that person’s health while they have been sequestered are included in quarantine protection. Cooperation of public health authorities, healthcare providers, and community leaders is needed for the implementation of effective quarantine measures aimed at maintaining compliance and reducing the social and economic effects of isolation.
Public Health Response
Lessons From Previous Outbreaks
Past lessons from the Nipah virus outbreak are analyzed to understand current public health strategies. In addition, past experiences remind us that rapid response, good communication, and sound surveillance systems are important for containing outbreaks. Early detection, community engagement, and international collaboration are also needed lessons learned. Implementing these insights strengthens preparedness and resilience against future Nipah virus crises and minimizes the chance of widespread transmission and extensive consequences.
Government Policies to Curb the Spread
Government policies have curbed the spread of the Nipah virus. Animal husbandry, food safety standards, and environmental management regulations mitigating zoonotic transmission risks are what these policies catch. Governments similarly invest in turning the cycle back to what it once was by building healthcare infrastructure to be equipped for handling any outrage that might occur. Campaigns in public health and education initiatives enhance community awareness and cooperation in preventive measures. A comprehensive response to Nipah virus threats must be done in the context of a coordinated and effective response based on comprehensive policy frameworks.
Global Efforts in Nipah Virus Control
Cross-border transmission of the Nipah virus requires a global effort to contain it. Research, surveillance, and response activities to manage outbreaks are coordinated among international organizations such as the World Health Organization and WHO. Countries can share shared data, resources, and best practices through collaborative initiatives. Vaccine development and distribution are supported through global partnerships that provide the protections vulnerable populations need. Coordinated action internationally to tackle Nipah virus-related problems creates the ability to have a multi-pronged and sustainable system that can be implemented at the local level.
Conclusion
Improvement of Nipah virus patient outcomes depends on early recognition and supportive care. The risks around the Nipah virus are severe, with respiratory and neurological symptoms. Spreading the virus can be prevented through good hygiene, safe animal handling, avoidance of contaminated foods and other precautionary measures.
Community awareness and vigilance are crucial to managing the Nipah virus crisis. This allows the educated population to follow proper preventive laws, identify early signs, and immediately seek medical care. Enhancing awareness and response as a collective effort adds value to public health resilience and significantly lowers the effect of Nipah virus outbreaks on communities worldwide.
FAQs
How Do You Know If You Have Nipah Virus?
If you develop fever, headache, and neurological problems and have known or suspected exposure to the Nipah virus, get medically evaluated to determine whether you have the virus. Confirmation requires diagnostic tests, primarily RT-PCR and serological assays.
Can the Nipah virus be treated successfully?
There is no specific treatment for the Nipah virus, however, but supportive care can help. To enhance survival chances, severe symptoms need to be managed with early medical intervention and intensive care.
Is There a Cure for Nipah Virus?
There is no cure for the Nipah virus. Treatment aims to provide supportive care to lessen symptoms and control complications. Great efforts are being made to find effective antiviral therapies and vaccines.
What Is the Mortality Rate of the Nipah Virus?
The mortality rate of the Nipah virus is very high, sometimes more than 70%. The rate depends on the outbreak context, access to medical care, and the severity of the infected's symptoms.
How Can I Stay Safe During an Outbreak?
During an outbreak, practice good hygiene, avoid contact with infected people, eat safe food, and follow public health guidelines. If necessary, wear protective gear and stay informed through reputable sources.